SCIMEA Works with People.cn and IFENG.COM to Jointly Promote Sichuan Experience on COVID-19 Treatment

Open the phone and scan
Recently, Sichuan International Medical Exchange & Promotion Association has worked with people.cn, Xinhua News Agency, IFENG.COM, dxy.cn, sina.com.cn, qq.com and other first-tier media to conduct a special report on the Sichuan experience on COVID-19 treatment:
The effective treatment of critically ill
patients with COVID-19 is the key to reducing the overall mortality. From
January 16 to March 15, 2020, a total of 539 diagnosed patients were treated in
Sichuan, 81 of which met the national criteria for medium severe and critically
ill patient standard specified in COVID-19 Diagnosis and Treatment Plan. Its 28-day
overall fatality rate is 0.6% (3/539), and the mortality rate of severe and
critically ill patients is 3.7%, which are lower than the domestic average
(overall mortality rate at 2.3%, and critically patient mortality rate at 8.1%)
and average of other parts of the world (overall global mortality rate at about
6%).
Initiated by West China Hospital, Sichuan
University, a total of 21 hospitals including Public Health Clinical Center of
Chengdu, West China Guang'an Hospital, Sichuan University, Ganzi People's
Hospital, etc., which participated in the treatment of critically ill patients
of Novel Coronavirus Pneumonia, and the Clinical Research Center of
the Shanghai First Maternity and Infant Hospital formed Study of 2019
Novel Coronavirus Pneumonia Infected Critically Ill Patients in Sichuan
Province, SUNRISE and conducted a follow-up and analysis on the above 81 cases
of severe and critically ill patients. The study shows that:
1. The median age of critically ill patients
in this group is 50 (39-65) years old, 37% of which are female, and 53.1% of
which have chronic comorbidities;
2. According to the national scheme for
clinical classification of medium severe and critically ill standards and daily
reporting system, all critically ill patients were identified before
intubation, where the oxygenation index <300 mmHg is the most sensitive one
of the five diagnostic indicators, and the sensitivity rate was 87.7%;
3. All critically ill patients are admitted to
the intensive care department of the designated hospital or the "temporary
ICU" established quickly to provide patients with necessary monitoring,
supportive equipment and critical care management team to ensure that all
critical patients could receive appropriate monitoring and treatment for
critical ill patients. 95.1% (77) of patients were transferred to ICU or
"temporary ICU" before or on the day of diagnosis of critically ill
patients. During the overall treatment, 63% (51) of critically ill patients
were treated in the "temporary ICU";
4. 76 patients (93.8%) received different
types of respiratory support treatment on the day of diagnosis as critically
ill patients, including 55 patients through traditional oxygen therapy (67.9%),
eight patients through nasal high-flow oxygen inhalation (9.9%), and 13
patients through noninvasive ventilation (16.1%). No patient needed invasive
mechanical ventilation or ECMO support on the day of diagnosis.
5. Throughout the treatment of critically ill
patients, traditional oxygen therapy is the most common respiratory support
(62.7%), followed by nasal high-flow oxygen inhalation (19.3%), noninvasive
ventilation (9.4%), invasive ventilation (8.5%), and ECMO (0.06%).
This study shows that under the current lack
of effective treatment drugs for COVID-19, Sichuan's treatment experience
suggests that early identification and timely provision of reasonable
respiratory support can keep the mortality rate of critically ill patients of
COVID-19 at a low level. In the early stage of critically ill patients of
COVID-19, close monitoring and traditional oxygen therapy should be the
recommended treatment measures in priority.
The research has been published on the
pre-printed platform of Medrix, with corresponding authors Professor Kang Yan
and Professor Jin Xiaodong of the Department of Intensive Care, West China
Hospital, Sichuan University.
(https://www.medrxiv.org/content/10.1101/2020.03.22.20041277v2.article-metrics)
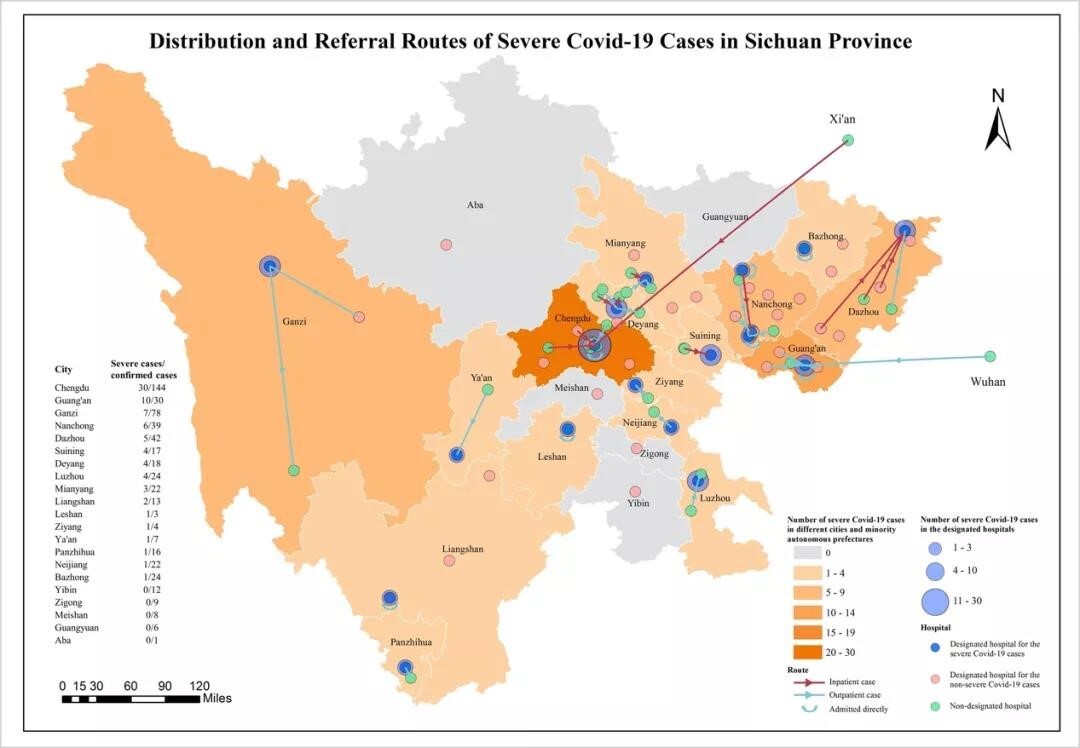
Figure 1. Distribution and transport map of
critically ill patients with COVID-19 in Sichuan Province
81 critically ill patients were distributed in 13 cities and two autonomous prefectures in Sichuan Province. The dark blue dots represent 18 designated hospitals that treated critically ill patients with COVID-19, the pink dots represent 30 designated hospitals that treated non-critically ill patients with COVID-19, and the green dots represent non-designated hospitals. The red and green arrows represent transfer and outpatient visits respectively. The figure shows the process of centralized management of critically ill patients.
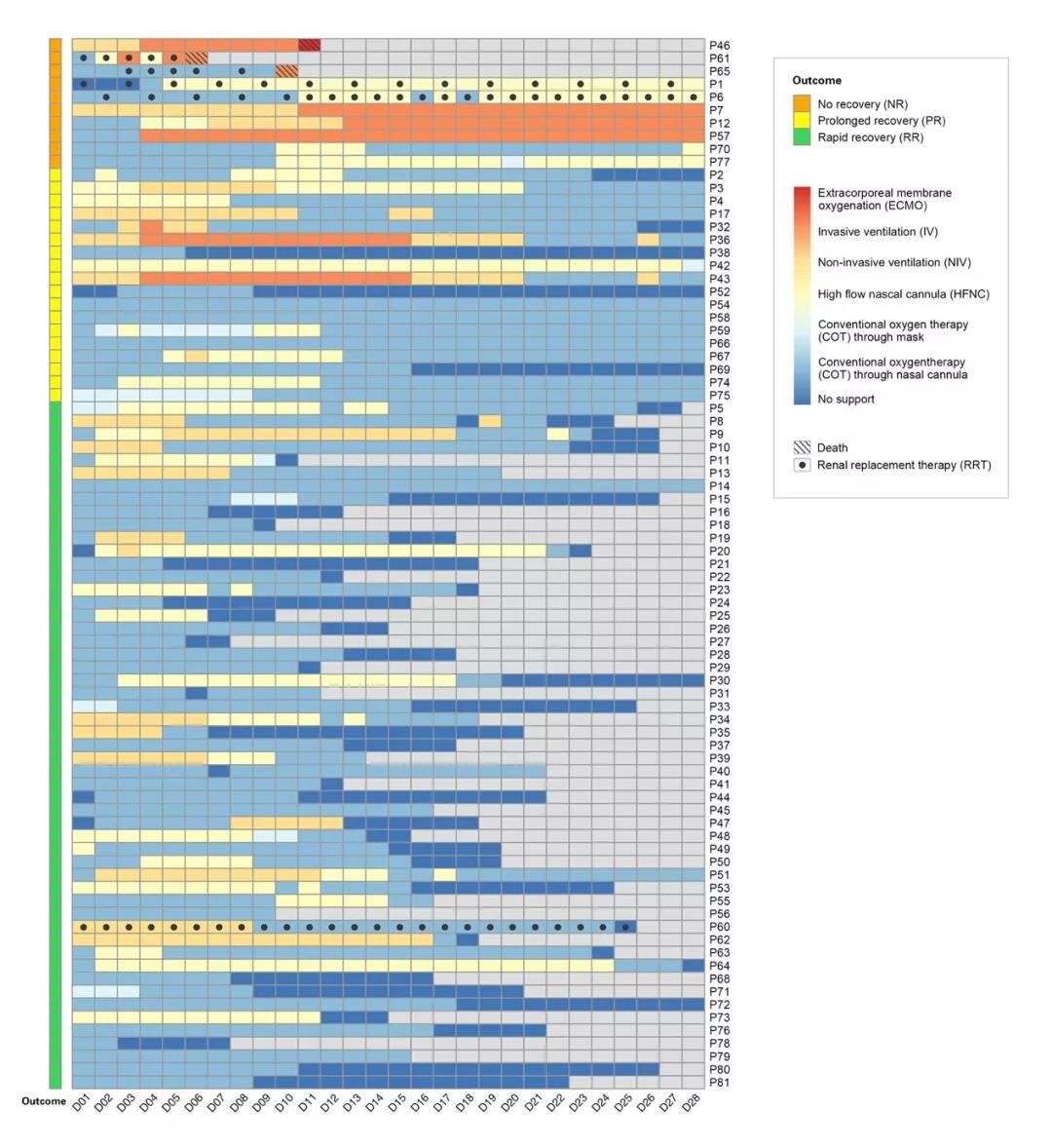
Figure 2. Daily vital organ function support
of 81 patients from the day of diagnosis as critically ill patients (D1) to the
28th day (D28).
This figure shows the daily respiratory
support and renal replacement therapy for critically ill patients of COVID-19
from D1 to D28.
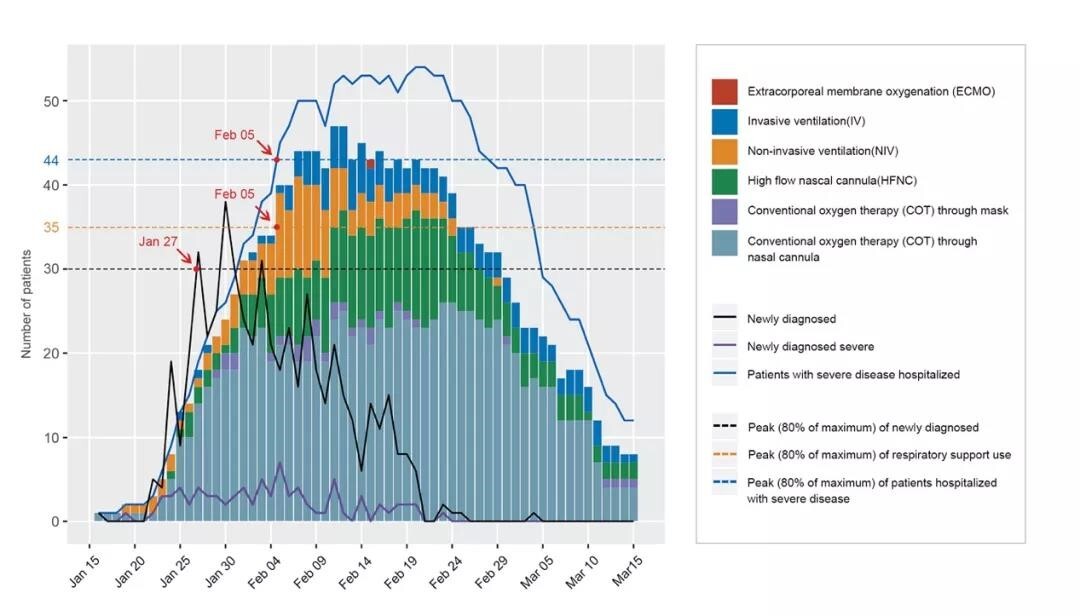
Figure 3. Respiratory support in critically
ill patients with COVID-19 during the study (January 16 to March 15).
The histogram represents the daily amount of
respiratory support. The black, purple, and blue lines represent the number of
new cases per day, the number of new critically ill cases per day, and the
cumulative number of hospitalized critically ill cases in Sichuan Province.